|
After being fouled in a basketball game, players find themselves at the free-throw line to take a shot. Overall, the shooting motion looks relatively similar among players, but there are small differences that make each player’s technique unique to them. If you watch closely, you may notice that each player has their own stance, pre-shot routine and shooting mechanics. A professional basketball player spends countless hours practicing this shot and developing a routine that makes them feel comfortable and confident. There’s a saying in neuroscience that’s applicable here: “Nerves that fire together, wire together.” With practice, their brain creates a crisp and fine-tuned program for shooting the free throw, and repetition makes approaching their shot second nature. The less thinking required for the actual shot mechanics, the less they’ll try to make small adjustments in response to stress, pressure, fatigue and fear that could interfere with making the shot. This ability of the brain to adapt, change, rewire and refine is referred to as neuroplasticity. The repeated experience of pain is fired and wired together similarly to practicing free throws. The more you experience, think about and focus on pain, the more you can improve your brain’s ability to activate that pain program. Just like the way practice refines the shooter’s skills, the more you expect and believe pain will occur, the more likely pain will actually occur.
Want More Analogies Similar to This One?For this analogy and 50+ others, I highly recommend checking out my new book with co-author Jarod Hall. The book is titled Sticks and Stones. It is a collection of analogies & stories to help people gain a deeper understanding of the complex nature of pain. With each analogy and metaphor covered throughout this text, you’ll find multiple stories that help relate the complex topics of pain, tissue breakdown, posture and more. Through each story, you’ll notice a strong focus on the power of language. Jim Heafner PT, DPT, OCS
Heafner Health Physical Therapy Boulder, Colorado
19 Comments
Sciatica, carpal tunnel, neuropathy...these words all have scary connotations! Fortunately, the majority of nerve-related symptoms are not threatening. Each of these diagnosis' are a symptom describing the specific tissue that is irritated. They do not address the underlying issues that cause the pain, nor how to treat it.For example, if someone comes into Heafner Health with wrist pain, and I identify they have carpal tunnel syndrome, I know the median nerve is receiving extra stress. While the compression or tension may be at the wrist (where the person is experiencing pain), the issue could be ANYWHERE along the nerve- in the neck, the shoulder region, forearm, or the wrist. Since the nervous system is a continuous structure, providing education about the nervous system and treatment anywhere along the nerve can result in a successful outcome! For this reason, understanding how nerves move and work can make a huge impact if you are experiencing pain. Nerves are like Garden Hoses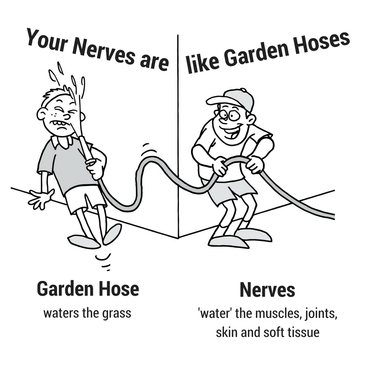 The nervous system functions similarly to a garden hose. Just as the garden hose delivers water, our nerves are responsible for feeding the muscles, joints, skin and other soft tissue. If the garden hose becomes kinked or compressed, the amount of water flowing through the hose is reduced. Your nerves respond in a similar fashion. If nerve pressure or irritation rises to a certain level, blood flow to the nerve and electricity through the nerve, known as the axoplasmic flow, is interrupted. This alters the amount of nutrition through the nerve and leads to an aggravated state. The nerve’s response to reduced nutrition can be a vague array of symptoms, most commonly described as numbness, burning, heaviness or tingling. To improve nerve nutrition, you must improve the flow of electricity and blood in the nerve. This is accomplished through gentle and specific movements and exercises. Fortunately, just as the garden hose returns to full function when the kink is released, nerves also respond favorably to the decreased compression and increased movement. -Jim Heafner PT, DPT, OCS Heafner Health Physical Therapy Boulder, Colorado
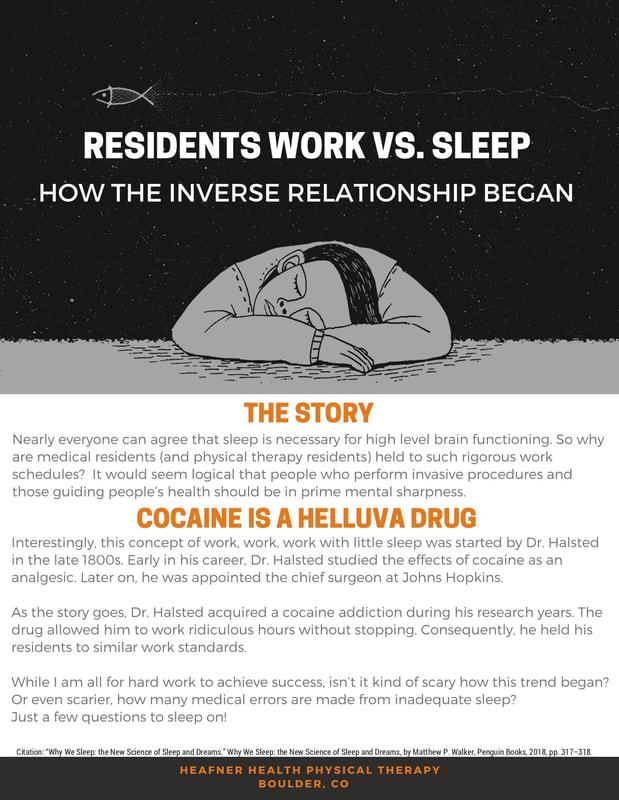
Recently, I have been fascinated with the subject of sleep, specifically the positive and negative health benefits of sleep.The research is overwhelmingly in favor of getting more sleep than not. According to the National Sleep Foundation adults need 7-8 hours of sleep each night (1). The good news: I am finally on board with this idea! I have dropped my old machismo ideations that I can force my way through fatigue. I know longer view exhaustion as an admirable, but rather an indication that my health is being compromised. The bad news: This is unfortunate and ironic timing considering I had my first child 6 days ago...! Regardless, I am finally prioritizing sleep. On my journey of learning about sleep, I ran across a fascinating story about medical residencies and sleep deprivation. More and more physical therapists are attending demanding residency programs! The physical therapy residency training model appears to be largely based off our close friend in the community: medical residents.In 2013, I graduated from the Harris Health System Orthopedic Residency program in Houston, Texas. Our program was tough, but our director, Dana Tew, did an excellent job mentoring my fellow residents and I on all aspects of life. We worked extremely hard at the clinic, but there was at least the opportunity of a work-life balance. Dana, who is also owner of the OPTIM Manual Therapy Fellowship, understood that our success and efficiency in the clinic directly correlated with our ability to sleep and manage stress outside the clinic. As I was going through my residency, my older brother, Tom was completing his general surgery residency. I recall him spending 30+ hours at the hospital on a regular basis. These long hospital shifts often had little (if any) sleep! Hearing this information, I thought to myself, "I would certainly rather have a surgeon at the beginning of a 30+ hour shift than the end. It has to be unsafe to perform a fine motor task that requires mental acuity after intense sleep deprivation." Who instituted these unattainable demands of high work and low sleep for people who need to in prime mental health to help others? The story is a quite interesting one! I would regularly ask myself, "Who instituted these unattainable demands of high work and low sleep for people who need to in prime mental health?"Citations:
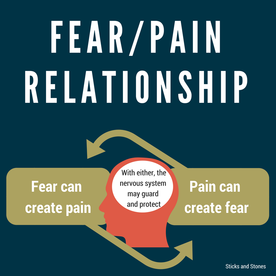
1. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary Hirshkowitz, Max et al. Sleep Health: Journal of the National Sleep Foundation , Volume 1 , Issue 1 , 40 - 43 From professional athletes to musical entertainers and beyond, high-energy performers execute complex motions with relative grace and ease. Whether it’s LeBron James dribbling down the court or Bruno Mars dancing on stage, their coordination and precision are due to the incredible motor control and movement pattern memory they’ve gained through countless hours of training. However, these well developed movement patterns can be altered in the presence of injury, fear, and more! At my clinic in Boulder, Colorado, I was recently working with a middle-aged man who was experiencing low back pain when lifting more than 40 pounds from the ground to the trunk of his SUV. This pain was interfering with his ability to perform work tasks as well as household chores. Within 3 treatment sessions, he was able to mimic the mechanics of the lifting motion without any pain. During visit 5, he performed the 40 pound lifting task repeatedly pain free. However, the following day at work, his pain immediately returned when attempting a lift. The above example, demonstrates the complexity of pain. This client objectively demonstrated proper strength and mobility to perform the lift in clinic; yet, when attempting the lift at work, the pain returned. When I asked him about the experience he said, "I don't know why it hurt at work...I felt tense as if my muscles were protecting me from the movement...I was anticipating the pain...Since I was injured at work, the lift scared me." At this point, I reminded him of the many factors, including fear, that can impact his experience of pain. "Fear and pain have a very intimate relationship"
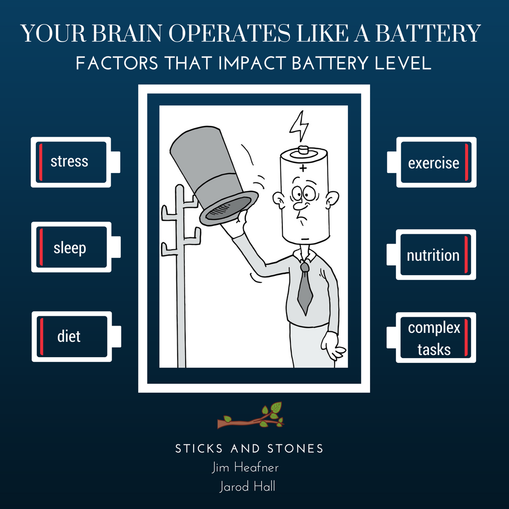
 Martial artist and actor Bruce Lee illustrated this idea beautifully: “You must be shapeless, formless, like water. When you pour water in a cup, it becomes the cup. When you pour water in a bottle, it becomes the bottle. When you pour water in a teapot, it becomes the teapot. Water can drip and it can crash. Become like water, my friend.” Water flows freely and fearlessly. Water doesn't stiffen or guard itself for protection. Water is smooth and fluid. Water is powerful. When learning how to move out of pain, you must challenge yourself to relax and allow your body to become like water! While this may sound funny or unrealistic, it is important to learn how to relax with movement. For precise movement to occur, certain muscles must activate, while others simultaneously relax. Practicing the ability to move without stiffness can bring awareness to the movement and create learning opportunities that strengthen the connection between your brain and muscles. When dealing with pain, do not forget about the contextual factors! Practice and repetition of movement will decrease the protective response from your nervous system and improve the mind-muscle connections! Dr. Jim Heafner PT, DPT, OCS Heafner Health Physical Therapy Boulder, CO  If you found this post interesting, check out the book Sticks and Stones written by Dr. Jarod Hall and myself! The ebook contains 50+ analogies and stories pertaining to pain and movement! Sticks and Stones will officially be available in early June 2018 at our site: theraPTeutic alliance. Pre-order the book at the lowest price today by using the promo code: WORDSMATTER I was recently working with someone who had neck pain after a mountain biking accident. During the evaluation, he reported hitting his head on the ground and experiencing a concussion during the accident. He stated "I am having difficulty remembering recent events and multi-tasking is near impossible! It's extremely frustrating!." Performing higher level tasks was easier in the morning and became progressively more challenging throughout each day. Additionally, he reported the desire to take naps throughout the day. When he questioned why his brain felt exhausted, I told him "It is because your brain operates much like a battery." (This text is adapted from "Sticks & Stones," a book by Jarod Hall PT, DPT, OCS and Jim Heafner PT, DPT, OCS. "Sticks and Stones" is in the final stages of development. Final versions of the text to be released to public in May 2018. Please reach out if you are interested in learning more information!) If you have persistent pain, recently had a surgery, or an injury (such as a concussion), your brain may be working in overdrive! In each of these scenarios it's not uncommon for patients to report that their brains feel tired early in the day, that they have trouble doing complex thinking tasks such as math, and even mix up their left from their right! Why does this happen? In situations like this you can liken your brain to a battery. This idea can be thought of in two separate ways. 1) You start each day at 100%, but quickly drain the battery each day |
| Like this post? Check out how Pain is like an Alarm System! |
Most people think pain is an indicator of the amount of tissue damage present in the body. The belief is that high amounts of pain equate to a large injury, and a small amount of pain equates to a small injury. However, through extensive research, it has been shown that pain has little correlation to the amount of tissue damage. For example, a paper cut may cause intense pain, while a broken bone may go unnoticed. In 2013, when Louisville basketball player Kevin Ware sustained a horrific leg fracture, he reported, "it was one of those things where I couldn't believe it. I honestly didn't feel the pain. It was more a shock."
"At the center of the alarm system is your brain, which beeps when it THINKS something is going wrong or is potentially dangerous."
Kevin Ware’s story perfectly demonstrates that pain is more like an alarm system. It is an evolutionary provided and naturally built system designed to keep you out of danger. At the center of the alarm system is your brain, which beeps when it THINKS something is going wrong or is potentially dangerous. If the system is healthy, it warns you when something is wrong just as your home alarm rings when a burglar breaks a window or your car alarm sounds if a car thief tries to wiggle your door open.
"Just as a smoke detector can be set off in the absence of fire, a home alarm in the absence of a burglary, and a car alarm when you accidently press the panic button, your body’s alarm system sounds off signals of pain in the absence of any REAL danger or threat."
However, just as a smoke detector can be set off in the absence of fire, a home alarm in the absence of a burglary, and a car alarm when you accidently press the panic button, your body’s alarm system sounds off signals of pain in the absence of any REAL danger or threat. The alarm may sound if a bird flies into a window or if you accidentally open the door after you have set the security code. In both of these cases there is no real danger, but the alarm rings in an effort to protect you. For safety, it is far superior for the alarm to be more sensitive and have false alarms, rather than to be hard to trip and not protect you in the case of a true threat.
Just as other alarms can misfire, your internal protective mechanism can do the same. Fear, stress, endorphins and adrenaline, anxiety, depression, lack of sleep, overactivity, poor nutrition, sickness, and many more factors can influence your alarm system’s perception of danger, increase sensitivity, and lead to a greater protective experience of pain. In Kevin Ware’s story, a large amount of endorphins and adrenaline as well as a massive NCAA crowd slowed his alarm system from signaling. Being familiar with the numerous factors that turn up or turn down the sensitivity of your internal alarm system is the first step in understanding how to better calibrate in the presence of injury.
Just as other alarms can misfire, your internal protective mechanism can do the same. Fear, stress, endorphins and adrenaline, anxiety, depression, lack of sleep, overactivity, poor nutrition, sickness, and many more factors can influence your alarm system’s perception of danger, increase sensitivity, and lead to a greater protective experience of pain. In Kevin Ware’s story, a large amount of endorphins and adrenaline as well as a massive NCAA crowd slowed his alarm system from signaling. Being familiar with the numerous factors that turn up or turn down the sensitivity of your internal alarm system is the first step in understanding how to better calibrate in the presence of injury.
(This text is adapted from "Sticks & Stones," a book by Jarod Hall PT, DPT, OCS and Jim Heafner PT, DPT, OCS. "Sticks and Stones" is in the final stages of development. Final versions of the text to be released to public in May 2018. Please reach out if you are interested in learning more information!)
If you think your pain-alarm system is misfiring, contact Heafner Health!
Does this Man have Arthritis?
Research shows that over 70% of people have arthritic changes, but not all of these people experience symptoms. While the man above likely has arthritic changes that could seen on an X-ray, these changes would be completely normal for his age. More importantly, it does NOT mean he has to be experiencing pain!
What is Osteoarthritis?
Arthritis is the leading cause of disability in the United States, and osteoarthritis (OA) is the most common form of arthritis. OA is a degeneration (breakdown) of the joint cartilage that can lead to stiffness and decreased range of motion at a joint. It is common in weight-bearing joints including the low back, hips, and knees.
What Osteoarthritis is NOT!
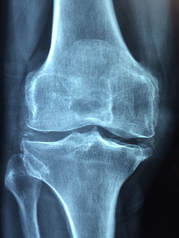
While the degenerative changes associated with OA do not directly cause pain, they are often blamed as the problem behind the symptoms. In reality, the signs and symptoms of OA are a natural aspect of the aging process. Several studies have been published over the past few years that confirm pain is not related to the natural wear and tear in our tissues. For example, 34% of asymptomatic people >60 years old have been found to have rotator cuff tears (1). Crazy right? One in three people WITHOUT SHOULDER PAIN have a rotator cuff tear. These natural body changes do not occur only in the shoulder, but throughout the entire body. Two out of four people WITHOUT KNEE PAIN have degenerative changes in their knees. (2)
Should these people sign up for surgery? I sure hope not. They do not even know there is an issue, and they are doing all of their activities without any problems. There would be no indication for surgery. These people should maintain an active and dynamic lifestyle. Therefore, we cannot confidently say that changes in our tissue are the source of pain or symptoms.
Should these people sign up for surgery? I sure hope not. They do not even know there is an issue, and they are doing all of their activities without any problems. There would be no indication for surgery. These people should maintain an active and dynamic lifestyle. Therefore, we cannot confidently say that changes in our tissue are the source of pain or symptoms.
Reframing How to Think about Osteoarthritis
OA is more closely related to the natural wear and tear that occurs in our joints as we get older. For example, think about your mother, father, grandmother, or grandfather. Over time they have developed wrinkles and other age-related changes. Despite these signs of aging, they do not complain about face pain from the wrinkles or scalp pain from their hair turning from dark to light. The same is also true for our wrinkles on the inside (3). We age on the inside in a similar fashion to how we age on the outside!
External Signs of Aging |
Internal Signs of Aging |
|
|
| See More from Heafner Health |
Action Steps
1) Get active! Have you ever heard the expression "motion is lotion" or "movement is medicine." These catchy sayings are true. One of the best things someone can do for arthritis is movement. At Heafner Health, we recommend a combination of flexibility and strengthening exercises to keep joints strong and mobile.
2) Diet and Weight Management. The Arthritis Foundation reports that "being just 10 pounds overweight puts an extra 30 to 60 pounds of pressure on the knees." (1) A small weight change have a big impact on the stress across your joints.
3) Visit a Doctor of Physical Therapy. Physical therapists are experts in joint mobilizations, movement eduction, exercise prescription, and pain management.
2) Diet and Weight Management. The Arthritis Foundation reports that "being just 10 pounds overweight puts an extra 30 to 60 pounds of pressure on the knees." (1) A small weight change have a big impact on the stress across your joints.
3) Visit a Doctor of Physical Therapy. Physical therapists are experts in joint mobilizations, movement eduction, exercise prescription, and pain management.
Heafner Health Physical Therapy is owned and operated by Dr. Jim Heafner in Boulder, Colorado.
References:
1) Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. The Journal of bone and joint surgery. American volume. Jan 1995;77(1):10-15.
2) Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC musculoskeletal disorders. 2008;9:116.
3) Obesity and Arthritis. (2017) Arthritis Foundation. 9, February. 2018. Web access:
https://www.arthritis.org/about-arthritis/types/osteoarthritis/articles/obesity-osteoarthritis.php
4) Term "Wrinkles on the Inside" was originally used by Dr. Tim Flynn
1) Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. The Journal of bone and joint surgery. American volume. Jan 1995;77(1):10-15.
2) Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC musculoskeletal disorders. 2008;9:116.
3) Obesity and Arthritis. (2017) Arthritis Foundation. 9, February. 2018. Web access:
https://www.arthritis.org/about-arthritis/types/osteoarthritis/articles/obesity-osteoarthritis.php
4) Term "Wrinkles on the Inside" was originally used by Dr. Tim Flynn
Overview
This article will cover central spinal stenosis (not lateral (foraminal) stenosis.
- Lumbar spinal stenosis is narrowing of the spinal canal in the low back
- Stenosis commonly occurs due to age, degenerative, and arthritic changes
- Symptoms may include lower back and leg pain, lower body numbness or tingling, difficulty walking upright, and clumsiness with walking
- Severe cases of spinal stenosis may result in the inability to control bowel and bladder function
What is It?
The spine or bodies backbone consists of 31 separate vertebrae. The spinal cord is a bundle of nerves that travel down the entire spinal column. Spinal stenosis occurs when there is narrowing of the spinal canal, limiting movement of the nerves.
Spinal stenosis can occur for multiple reasons, but is primarily due to age related changes, such as arthritis. For this reason, spinal stenosis is more commonly seen in individuals over 50 years of age. Other less common causes of stenosis include spinal fracture, tumors, or other trauma to the spine.
Spinal stenosis can occur for multiple reasons, but is primarily due to age related changes, such as arthritis. For this reason, spinal stenosis is more commonly seen in individuals over 50 years of age. Other less common causes of stenosis include spinal fracture, tumors, or other trauma to the spine.
Symptoms of Spinal Stenosis
Since a major cause of spinal stenosis is osteoarthritis, symptoms typically develop gradually over time. Early on, individuals will complain of back pain, stiffness in the legs and thighs, and periodic numbness or tingling. Additionally a loss of sensation may be noted in the thighs or feet. As symptoms progress, gradual weakness or ataxia (incoordination) may be noted while walking. Typically, individuals with spinal stenosis feel better when leaning forward while performing activities. Bending forward creates more space in the spinal canal and decreases pressure on the nerves.
As spinal stenosis progresses, the severity of symptoms typically progress as well. For this reason, it is beneficial to seek medical care when you start noticing symptoms.
As spinal stenosis progresses, the severity of symptoms typically progress as well. For this reason, it is beneficial to seek medical care when you start noticing symptoms.
Treatment of Spinal Stenosis
While treatment is varied across the country, most individuals with lumbar stenosis should receive conservative management (physical therapy, NSAIDS, injections) prior to more serious medical interventions. A 2015 study by Dr. Delitto and colleagues found that surgery compared to nonsurgical treatment of lumbar spinal stenosis yielded similar long-term results. This profound study has shown that surgery is not necessary (or at least not needed as commonly) if you are suffering from lumbar stenosis.
At Heafner Health, I was recently working with someone diagnosed with moderate central spinal stenosis. During the initial evaluation, the client said, "normally I do not pay out of pocket, but this is my last option before surgery. I have had pain for 6 years without any relief from stem cell or steroid injections." This individual had pain every morning while getting out of bed. His symptoms would naturally lessen throughout the morning, but any prolonged sitting or walking increased his leg symptoms and affected his ability to work. Each evening his sense of stiffness returned, forcing him to take a muscle relaxer and CBD cream. Our sessions focused on a mobility approach, meaning we focused on the mobility of his spine and hips more than anything else. Within 6 sessions, he is no longer having leg pain during the day, and his morning stiffness decreases in minutes! While it is nice to show off our successes, more importantly it speaks to the point that surgery is not necessary. The proper interventions on a motivated patient will work!
While this approach will be different from individual to individual, a good physical therapy routine should consist of trunk strengthening exercises, decreasing pain and nerve symptoms, maximizing endurance, and lower extremity flexibility exercises. For a full review of lumbar spinal stenosis, I highly recommend reading the American Physical Therapy Associations article on Physical Therapists Guide to Lumbar Spinal Stenosis.
-Dr. Jim Heafner PT, DPT, OCS
Owner at Heafner Health Physical Therapy
At Heafner Health, I was recently working with someone diagnosed with moderate central spinal stenosis. During the initial evaluation, the client said, "normally I do not pay out of pocket, but this is my last option before surgery. I have had pain for 6 years without any relief from stem cell or steroid injections." This individual had pain every morning while getting out of bed. His symptoms would naturally lessen throughout the morning, but any prolonged sitting or walking increased his leg symptoms and affected his ability to work. Each evening his sense of stiffness returned, forcing him to take a muscle relaxer and CBD cream. Our sessions focused on a mobility approach, meaning we focused on the mobility of his spine and hips more than anything else. Within 6 sessions, he is no longer having leg pain during the day, and his morning stiffness decreases in minutes! While it is nice to show off our successes, more importantly it speaks to the point that surgery is not necessary. The proper interventions on a motivated patient will work!
While this approach will be different from individual to individual, a good physical therapy routine should consist of trunk strengthening exercises, decreasing pain and nerve symptoms, maximizing endurance, and lower extremity flexibility exercises. For a full review of lumbar spinal stenosis, I highly recommend reading the American Physical Therapy Associations article on Physical Therapists Guide to Lumbar Spinal Stenosis.
-Dr. Jim Heafner PT, DPT, OCS
Owner at Heafner Health Physical Therapy
References:
Delitto A, Piva SR, Moore CG, et al. Surgery versus nonsurgical treatment of lumbar spinal stenosis: a randomized trial. Ann Intern Med. 2015;162(7):465-473
Delitto A, Piva SR, Moore CG, et al. Surgery versus nonsurgical treatment of lumbar spinal stenosis: a randomized trial. Ann Intern Med. 2015;162(7):465-473
"MRIs can paint a scary picture! Fortunately in many instances, degenerative disc disease (DDD) is NOT as daunting as it sounds. Physical Therapy should be the first line of defense in treating DDD."
-Dr. Jim Heafner PT, DPT, OCS
Overview
- Degenerative Disc Disease (DDD) is commonly referred to as osteoarthritis or arthritis
- DDD is a natural aspect of aging, but can also occur due to a traumatic injury
- MRI studies have found many people without any pain or low back problems to have DDD. This means that DDD does not cause pain!
- In many instances, it is not the cause of a person’s pain. It is only a symptom!
- Long term studies show equal outcomes between conservative treatment and surgery
What is Degenerative Disc Disease (DDD)
The spine is made of 24 vertebrae and divided into three separate regions. The lowest of the three regions is known as the lumbar spine or low back, which has five vertebrae. Between each vertebrae there is a dense piece of connective tissue called a disc. DDD is degeneration of one or multiple discs in the spine.
Currently scientists and researchers have not identified a single cause of DDD; however, they have found several predisposing factors. First, DDD is thought to be a natural progression of age. Much like the body ages externally, it will also age internally. DDD has been compared to the wrinkles on one’s face or the gray hair that develops over time. Second, DDD may occur after a traumatic injury such as a bicycle accident or motor vehicle wreck. A traumatic injury is thought to expedite the degenerative process and potentially predispose a person to early arthritis. Finally, factors such as smoking have been linked to DDD. Smoking decreases the oxygen supply to the discs and does not promote proper nutrition or healing of the disc.
Currently scientists and researchers have not identified a single cause of DDD; however, they have found several predisposing factors. First, DDD is thought to be a natural progression of age. Much like the body ages externally, it will also age internally. DDD has been compared to the wrinkles on one’s face or the gray hair that develops over time. Second, DDD may occur after a traumatic injury such as a bicycle accident or motor vehicle wreck. A traumatic injury is thought to expedite the degenerative process and potentially predispose a person to early arthritis. Finally, factors such as smoking have been linked to DDD. Smoking decreases the oxygen supply to the discs and does not promote proper nutrition or healing of the disc.
Symptoms of DDD
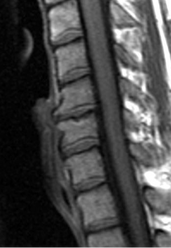
Individuals with DDD often have a gradual onset of low back pain. Symptoms may be located in the midline of the back or isolated to one side. Pain is often described as dull or achy and generally greater in the morning. Since DDD is often a natural aspect of aging, many individuals often have several episodes, each with a different duration of time. Pain and stiffness is more likely to be present after resting in a prolonged posture or performing a repetitive activity.
If symptoms of DDD worsen, pain can spread to the buttock or thighs. In these instances, other structures of the spine such as the nerves or muscles, may be receiving extra stress.
If symptoms of DDD worsen, pain can spread to the buttock or thighs. In these instances, other structures of the spine such as the nerves or muscles, may be receiving extra stress.
Treatment of DDD
Degenerative Disc Disease is commonly treated conservatively with a combination of physical therapy and NSAIDs. The goal of these treatments should be to minimize pain and gradually return people to their normal activities as quickly as possible. A quality rehabilitation program should include a combination of joint manipulation, core and hip strengthening exercises, spinal mobility exercises, and aerobic conditioning. Research has shown little effectiveness for modalities such as TENS or ultrasound.
If conservative management fails, an orthopedic surgeon or neurosurgeon will make the decision to perform more aggressive interventions. Individuals who require surgery often have advanced symptoms and debilitating pain. Patients should be aware that long term outcomes of conservative management and surgery are similar at a 10-year follow-up of patients with degenerative disc disease.
If conservative management fails, an orthopedic surgeon or neurosurgeon will make the decision to perform more aggressive interventions. Individuals who require surgery often have advanced symptoms and debilitating pain. Patients should be aware that long term outcomes of conservative management and surgery are similar at a 10-year follow-up of patients with degenerative disc disease.
For questions or treatment advice, call Heafner Health Physical Therapy.
(Heafner Health is located in Boulder, Colorado 80301)
Overview
- Muscle strains are a common source of low back pain
- Muscles spasms are a common symptom of irritated or strained low back muscles
- A combination of gentle, pain free movement and a gradual return to activity are important components of rehabilitation
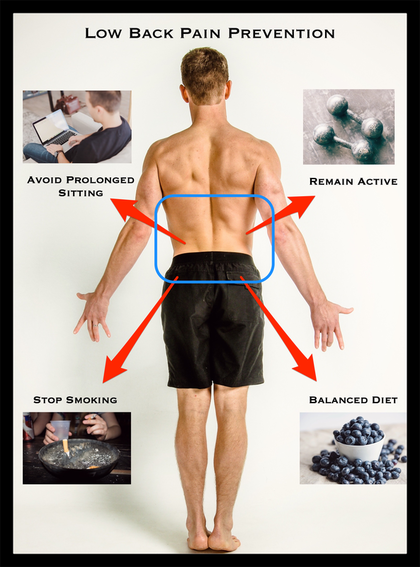
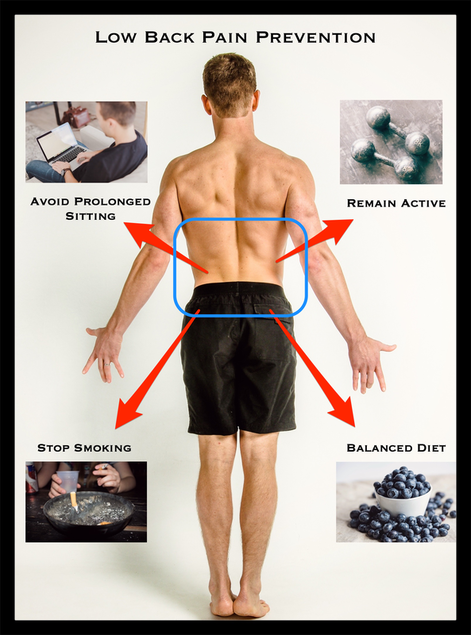
What is a Low Back Muscle Strain The muscles of the low back play an important role in both moving and supporting the spine. For example, the muscles must allow the spine to move when bending forward to lift a weight, and simultaneously protect the spine from excessive stress. Whenever the muscles are stretched too far or too quickly, an injury may occur. For this reason, bending, lifting, and twisting with poor body mechanics and poor preparation for movement may increase one’s risk of injury. Additionally, inactive people and smokers are at a higher risk of straining the low back muscles. |
Muscle Strain Symptoms
Following a low back muscle strain, people will often experience localized pain in the region of the strain. Spine and hip range of motion will likely be restricted as these movements can stress the injured area. Even simple motions such as rolling in bed or moving from sit to stand can cause significant strain. In an isolated muscle strain, the individual should not notice any neurological signs (numbness, tingling, muscle atrophy, or other symptoms down the legs).
Muscle Strain Treatment
| Treatment of a low back muscle strain will be similar to muscle strains throughout the body. In the first few hours to days following the injury, gentle pain free movements are very important. The acronym ‘POLICE’ is a great strategy to recall the important steps following a muscle strain.
|
Additionally, it is recommended to see a Doctor of Physical Therapy within the first several days following a lumbar injury. The Physical Therapist can help decrease pain and more importantly prevent injury from occurring in the future.
Bonus Treatment Advice
For previous articles on low back muscle strains, please read the following blog posts!
| About Heafner Health: Heafner Health Physical Therapy is owned and operated by Dr. Jim Heafner. His evidenced-based treatment approach is different than your average physical therapist. As a residency trained Orthopedic Specialist, Jim identifies the cause of people’s pain and symptoms. His treatments combine hands-on techniques (including soft tissue work and adjustments) as well as corrective exercises, with the goal of getting people back to the activities they enjoy most. Jim strongly believes that pain is not permanent, and everyone should have the opportunity to be strong and healthy throughout their entire life. Heafner Health is conveniently located inside RallySport in Boulder, Colorado. All treatment sessions are 1-on-1. We treat everyone from top athletes to weekend warriors. No doctor’s referral is required prior to evaluation! Stop managing your pain and start your path to wellness. Learn more at www.heafnerhealth.com |
Heafner Health
Physical Therapy
Manual Therapy
Movement Specialists
Pain Management
Archives
April 2024
February 2024
January 2024
June 2023
April 2022
October 2019
February 2019
September 2018
August 2018
July 2018
June 2018
May 2018
March 2018
February 2018
January 2018
December 2017
November 2017
September 2017
August 2017
July 2017
June 2017
May 2017
April 2017
March 2017
January 2017
September 2016
August 2016
July 2016
June 2016
May 2016
April 2016
March 2016
February 2016














 RSS Feed
RSS Feed
